Midwestern University, Arizona College of Optometry
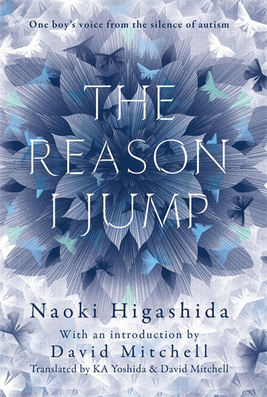
The Reason I Jump offers an insiders guide to the autistic experiences of a non-verbal Japanese thirteen year old, Naoki Higashida. It was first published in 2007 and has since been translated into over 24 languages. The novel is presented as a Q & A, with brief short stories in between serving as coffee breaks for the reader. Higashida is able to answer via an alphabet grid constructed specially for him. There is also an introduction/preface and afterword by David Mitchell, shedding a little more light as to how this New York Times Bestseller came to fruition.
Mitchell explains that the aim of the novel is to demonstrate that those diagnosed with autism continue to possess intellectual acuity and spiritual curiosity. He also wanted to discredit the thought stream that autistic individuals are “antisocial loners who lack empathy.”
I think the novel accomplished all of its goals and more. It becomes evident in his extremely personal answers that Higashida is a deeply thoughtful and spiritual individual. When asked if he would like to be “normal” (Q24), Higashida says “I’ve learnt that every human being, with or without disabilities, needs to strive to do their best, and by striving for happiness, you will arrive at happiness.” He continues, “as long as we can learn to love ourselves, I’m not sure how much it matters whether we’re normal or autistic.” His answers are deep, complex and sympathetic, often stating “ please, whatever you do, don’t give up on us. We need your help.” (Q5) Perhaps the greatest lesson to take away form this book was stated by David Mitchell in his forward. He said, “ emotional poverty and an aversion to company are not symptoms of autism but consequences of autism.” As Higashida explains in Question 13, “because things never, ever go right, we end up getting used to being alone, without even noticing its happening” and “whenever I overhear someone remark how much I prefer being on my own, it makes me feel desperately lonely.” His experiences and explanations are not always relatable but are eye opening to minds of individuals who march to the beat of their own drum.
I would recommend this book to both health care professionals and the general public because of the importance of the message it is trying to convey. His hardships are not unique and can offer insight into thought processes different than our own. When describing unpleasant flashbacks that lead to emotional meltdowns, Higashida says “please try to understand what we’re going through and stay with us,” which is a recurring statement he makes throughout the interview. To the reader, this is a neon sign that says we need more compassion and understanding in our society.
Today, Higashida continues to act as an advocate for autism. He keeps an informative blog and is regularly featured in Japanese magazine The Big issue. He has continued to write several poems, essays and novels and is now twenty-four years old.


 RSS Feed
RSS Feed

